Male Fertility Overview
Infertility is a common condition and current estimates suggest that one in eight couples may have difficulty conceiving. Infertility is identified when a couple has been having unprotected intercourse (i.e. without any form of birth control) for 12 or more months, and pregnancy has not developed.
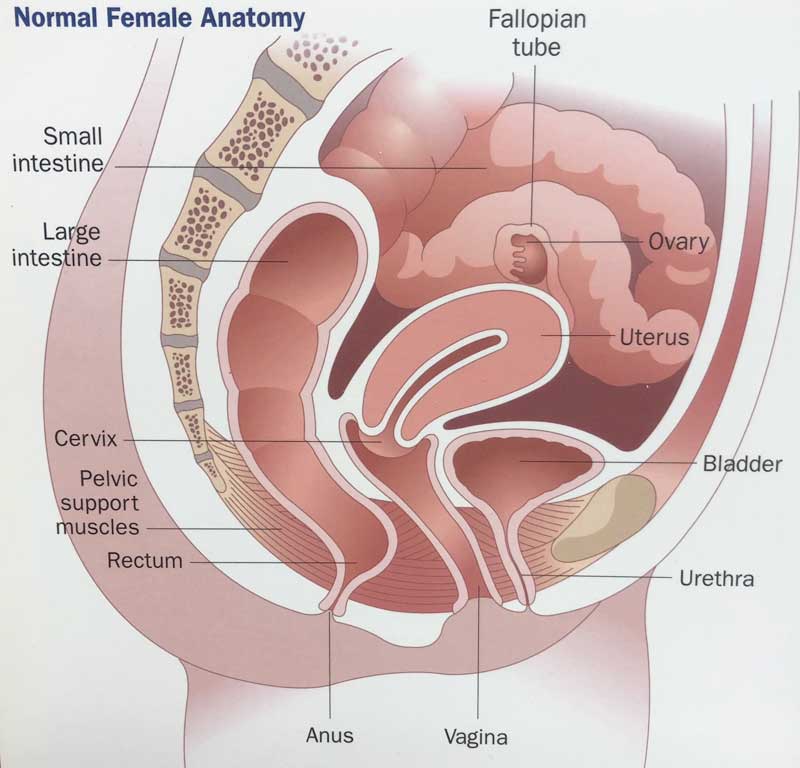
To understand evaluation for fertility, it helps to begin with a review of the reproductive process. On the female side, eggs are developed in the ovary. In normal circumstances, a woman ovulates once a month at mid cycle.
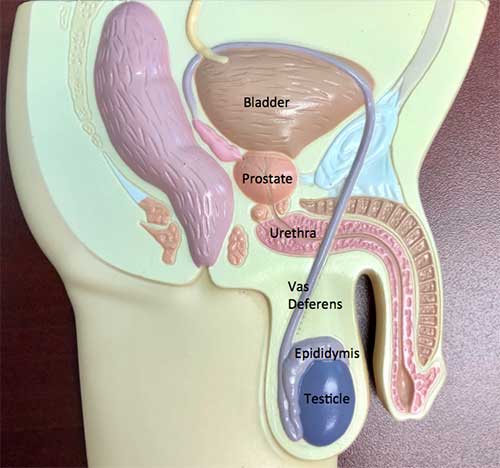
On the male side, sperm are constantly being made in the testis. Sperm, once made in the testis, travel through a series of tubes called the epididymis and vas deferens, to mix with fluid from the seminal vesicle and prostate to make the semen, which is released at ejaculation.
For fertilization to take place, sperm must make the journey from the vaginal area through the uterus (womb) and fallopian tube to fertilize the egg as it is released from the ovary. The egg, once fertilized, then travels through the tube to the uterus, where it implants in the uterus to begin pregnancy.
There are a variety of reasons that the reproductive process may not work. Current estimates suggest there may be a male factor in 20% of cases, and a male component contributing to a couple factor in another 20-40% of cases.
There are some general measures a couple can pursue to increase the chance for pregnancy. A woman can watch her cycle to determine when she ovulates with the use of temperature monitoring or an ovulation predictor kit (available over-the-counter in drug stores). The couple should have intercourse every day or every other day around the time of ovulation (but not more often, which may deplete the sperm count).
When pregnancy is not occurring, then urologic evaluation of the male begins with the medical history, during which questions are asked about sexual function to confirm that erection and ejaculation are working as intended. Physical exam is carried out to assess testicular size and consistency, to evaluate the presence of the epididymis and vas deferens, and to determine if varicocele (a dilated or varicose vein in back of the testicle) may be present.
The cornerstone of evaluation is the semen analysis. Semen is collected by ejaculation into a specimen cup. The sample is then examined within a select time period, usually within 30 minutes. Typically, the semen analysis needs to be done by a lab with particular expertise in the evaluation process, and cannot be routinely done by a general lab. The semen analysis is analyzed for a variety of factors, the main three of which are the sperm count (the number of sperm), the sperm motility (the percent of active sperm), and sperm morphology (the number of “normal” or mature sperm). (There are always some “abnormal” or immature sperm in every ejaculate.)
Other initial studies may be done to evaluate for a male factor contributing to infertility. On occasion, levels of hormones associated with sexual function in the reproductive process – testosterone, prolactin, luteinizing hormone (LH), and follicle stimulating hormone (FSH) – may be checked. Additionally, there are new genetic tests which may be checked in the scenario of very low sperm counts. In some cases, a scrotal ultrasound may be done to confirm if varicocele may be present, or to exclude the presence of an abnormality within the testicle if there is a concern raised by the physical exam.
When abnormalities on semen analysis are identified, there are some underlying issues that can be addressed by a urologist. If infection is present, that can be treated with an antibiotic. If a varicocele is present and it is interfering with semen quality (causing a “stress pattern” characterized by decreased count, low motility, and a decreased number of normal forms), then surgical repair of the varicocele may provide benefit. If there is obstruction of the tubes (which may occur if there has been prior surgery, such as vasectomy), surgical repair may help.
There are some general measures men can follow to improve semen quality. They should avoid substances that interfere with sperm production, which can include marijuana or alcohol in excess amounts. Increased temperature around the testis may interfere with sperm production, which leads to the generally recognized admonition to avoid hot tubs, and perhaps wear boxers instead of briefs.
Oftentimes during evaluation, it is noted that there is impaired semen quality, but there is not an underlying urologic issue to be fixed. In those circumstances, there may be impaired production of sperm that is occurring at the cellular level within the testis. With that recognition, efforts have been made for years to find medications that might boost or improve sperm quality and production, but the search remains elusive. Of anecdotal interest, the supplement Proxeed (available at proxeed.com) may provide benefit for some.
Even though there may not be remedies to improve sperm quality and count, current practice provides the opportunity for pregnancy through assisted reproduction. A full discussion of the details of assisted reproduction is beyond the scope of this newsletter, but to put forth the concept in general, if oversimplified terms, is the idea that if a single sperm is available it can be used to fertilize a single egg, which then can be implanted in the uterus. Sperm can be surgically retrieved from the testis and epididymis (see ICSI newsletter) for this process. Couples are best served by undergoing evaluation by physicians with particular expertise in assisted reproduction.
In summary, when a couple begins evaluation for fertility, the male partner may undergo evaluation by a urologist, who can begin the initial process to determine if there is an underlying urologic issue which may be addressed, or to help the assisted reproductive physician with techniques available (ICSI) to harvest sperm when needed.
Additional Information
Contact us to request an appointment or ask a question. We're here for you.



