UroLift Procedure BPH
The Urinary System
The urinary system begins with the kidneys, which make urine that runs through tubes down to the bladder. The bladder’s job is to store urine until full, then empty to the outside through the urethra, which is the pathway to the outside.
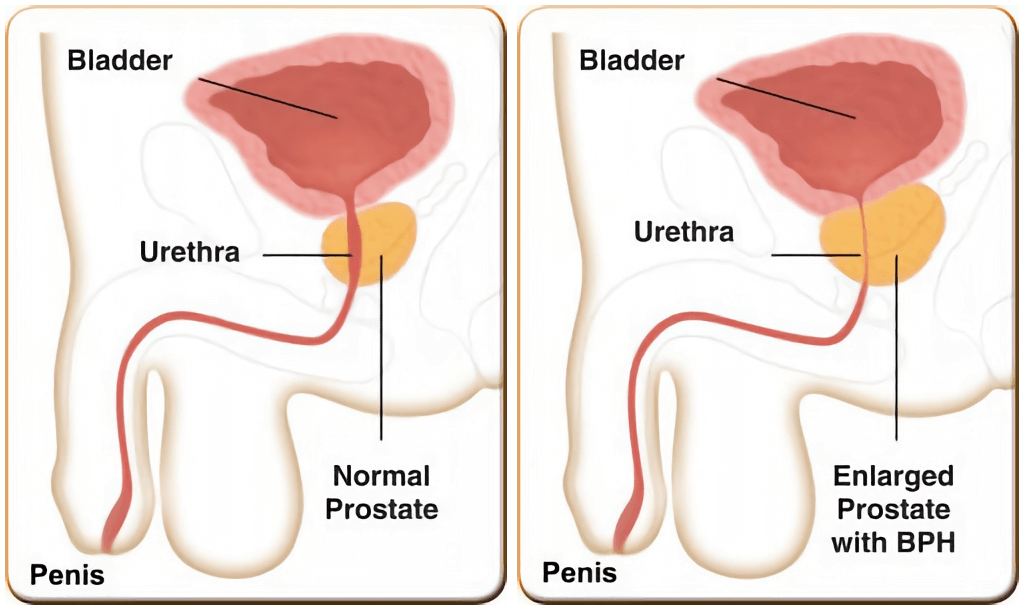
The prostate is the first part of the pathway. When men are 20, the pathway is wide open. When men reach the age of 40, the pathway begins to get blocked as the prostate enlarges. The prostate enlarges in most men (known as benign prostatic hyperplasia, or BPH).
If the enlarged prostate is not causing symptoms, it can be left as is. If the prostate enlarges and “blocks the pathway”, causing urinary bother, then an effort can be made to help lessen the burden associated with the change in urination.
When deciding what type of treatment should be used to help lessen the bother associated with the urinary changes, it is useful to look at the benefits and burdens of each of the different treatment avenues. Pills are often used as the first choice. In broad terms, there are two types of medication. The first type, the alpha blockers, open the pathway by relaxing the outer grip of the prostate. The second type, Proscar (finasteride) and Avodart (dutasteride), reduce the size of the enlargement, and can lead to less blockage after a period, usually 6 to 12 months. For some men, medications do not provide enough relief. For other men, they do not like having to take pills on an ongoing basis. If medications are not the answer, there are different techniques available to open the blocked pathway.
Common Techniques
The most commonly used techniques, greenlight laser and TURP, are very effective ways to open the pathway to relieve the obstruction. These procedures require a general anesthetic, and a catheter that stays in for 2 to 3 days after the procedure. Both of those procedures can cause retrograde ejaculation, also known as dry climax. In that circumstance, semen is still produced, but at the time of climax, it back washes up into the bladder, rather than coming out the tip of the penis with ejaculation.
New techniques, known as minimally invasive procedures seek to provide a less invasive way to open the pathway. From the patient standpoint, a successful technique is one that it is easy to tolerate, improves urinary symptoms, allows a quick return to normal activities, poses minimal hazards that can occur as a result of treatment and one that can be done at a manageable cost.
The goal of these techniques remains the same – address the blocking part of the prostate, open the urinary pathway, and allow improved urinary flow.
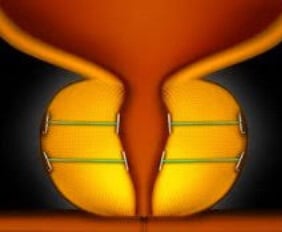
The UroLift implant is placed using the cystoscope, the fiberoptic catheter used to look in the urethra and the bladder. The procedure, done with IV sedation, does not require a full general anesthesia.
The Advantages of the UroLift Procedure
The advantages of the UroLift procedure are that it may allow one to stop taking pills for the enlarged prostate, it can avoid the potential hazards that may occur with one of the more invasive procedures, and it typically does not require an overnight stay. Most men do not require a catheter after the procedure. Sexual function remains the same, and ejaculation is usually preserved.
Again, a useful format to understand the approach to the enlarged prostate, is to be aware of the different tools which are available to help, and to view those tools in the context of potential benefits and burdens. The ideal outcome is to find the treatment avenue that offers the most benefit while minimizing potential burdens.
What tests are needed to see if UroLift is for me?
To determine if a man is a candidate for the UroLift procedure, the following two tests must be done.
First, the size of the prostate has to be measured with ultrasound (or some other imaging study such as CT or MRI). The prostate has to be less than 100 cc in size to be treated with the Urolift technique.
Second, the urinary pathway, prostate and bladder need to be examined with office cystoscopy. The anatomy of the blockage caused by the prostate needs to be assessed to see if the Urolift technique will work.
Why do I need a cystoscopy? Does it hurt?
If there is “side to side” blockage of the pathway by the prostate, UroLift can be carried out. If there is a “middle lobe“ which causes the blockage, the urolift technique may not be suitable.
Although it sounds intimidating, office cystoscopy is a straightforward procedure. A numbing gel is placed in the urinary pathway. The cystoscope (a fiber optic catheter) is advanced into the urinary bladder. The procedure takes less than 60 seconds. Men worry whether it will be painful, but most note the main bother is only the 10 second sensation of the strong need to void when the catheter is first passed into the bladder.
Are there any other things that need to be done?
A third step that may be carried out to evaluate a man as a candidate for the UroLift is to keep a voiding diary. The patient measures the time and amount of each void. This provides information about the capacity of the bladder (how much does the bladder hold), and it also allows an assessment of the volume of urine produced, during both the day and the night.
For frame of reference, the bladder normally holds 300 to 400 mL (10 to 14 ounces). The normal amount of urine production is 1500 to 2000 mL (50 to 65 ounces) in a 24-hour period.
When a man is in his 20s, the amount of urine produced over night is typically only about 200 to 300 mL (with normal bladder capacity, the bladder does not fill up overnight). By the time men reach age 40, the amount of nighttime urine production can increase considerably, and in some cases there may be over 1000 mL of urine produced at night (it is this increase in the volume of urine production, in association with a reduced bladder capacity, that may cause a man to get up more frequently at night to void).
Where is the procedure done? Am I awake? Will I need a catheter?
The UroLift technique is done as an outpatient at the surgery center. It takes about 10 minutes. It is done with IV sedation (IV sedation is the same type of anesthesia used for procedures such as a colonoscopy).
Some men are able to void right after the procedure and do not need a catheter. About half of the men may require a catheter for a day, or several days, after the procedure.
What happens during recovery?
Men can resume all of their normal activities following surgery, but should avoid heavy yard work or gym activity for 2 weeks.
During the first few weeks, there may be increased urinary bother including more frequent urination, a sense of urgency, blood in the urine, and discomfort with urination. Those symptoms typically resolve after a few weeks.
The first goal to look for postoperatively is improved urinary flow. Once the bladder is able to empty more freely, and does not have to work as hard to push urine out against obstruction, it may begin to regain its elasticity. As it regains its elasticity, it can store increased volumes (it can hold more), which may then reduce the symptoms of frequency, urgency, and increased number of nighttime urinations.
Take home message
In summary, UroLift has been a great addition to the treatments available to help improve urination in men who have difficulty with a large prostate.
Dr. Christine Tran and Dr. Nathan Roberts have a Center of Excellence (COE) for UroLift
Dr. Nathan Roberts from The Urology Group in Lansdowne, VA has been designated as a UroLift Center of Excellence (COE). Physicians achieving designation as a UroLift COE have achieved a high level of training with the UroLift System and demonstrated a commitment to care for men suffering from symptoms associated with Benign Prostatic Hyperplasia (BPH), also known as enlarged prostate.
Dr. Tran (BPH & The Role of Minimally Invasive Treatments)
Contact us to request an appointment or ask a question. We're here for you.



