Active Surveillance for Localized Prostate Cancer
Prostate cancer is the most common type of non-skin cancer in men and is the second leading cause of cancer death in men.
What is PSA? How is it used to diagnose prostate cancer?
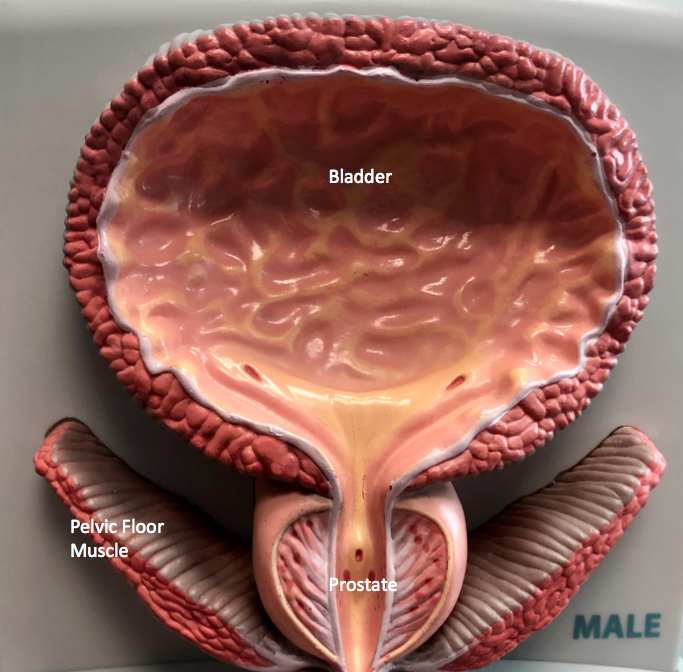
Since the 1990s, PSA has been routinely used as a screening test for prostate cancer. PSA, which stands for prostate specific antigen, is a protein made only in the prostate and not elsewhere in the body. Elevation of the PSA is nonspecific, and may occur due to the age appropriate prostate enlargement (benign prostatic hyperplasia, or BPH), inflammation, or it may be the first sign of prostate cancer.
The standard of care to evaluate an elevated PSA has included prostate ultrasound and prostate biopsy, which has led to a marked increase in the number of men diagnosed with prostate cancer.
When prostate cancer is diagnosed, does it always need treatment?
Of all those men who are diagnosed with cancer, a subset will have an aggressive type disease that if left untreated, will progress with cancer spread beyond the prostate and which may eventually cause death from prostate cancer.
For those men who have aggressive disease, intervention with surgery (radical prostatectomy) or radiation (either external beam radiation or brachytherapy, also known as seed implant) addresses the prostate cancer in an effort to cure the prostate cancer or reduce its potential for subsequent spread. However, both of those treatment avenues pose potential hazards, which can include ED (loss of erection), or incontinence (unwanted urinary leakage).
Are there some types of prostate cancer that do not need treatment?
A significant proportion of men with prostate cancer will have less aggressive disease, with a type of cancer that follows a more indolent course, which means it is likely to stay confined within the prostate and not spread to other sites or cause prostate cancer death. With the recognition that many men have disease that will not progress, and that the treatment avenues of surgery and radiation pose the risk of potential hazards, current practice allows those men with low risk disease to be treated with active surveillance, with serial monitoring of the disease, with plans for intervention if the disease shows signs of progression.
Why use active surveillance for prostate cancer?
As noted in the American Urology Association (AUA) Guidelines, “a program of active surveillance is based on the premise that some, but not all, patients may benefit from treatment of their primary prostate cancer. A program of active surveillance has two goals: (1) to provide definitive treatment for men with localized cancers that are likely to progress and (2) to reduce the risk of treatment-related complications for men with cancers that are not likely to progress.”
Which men have low risk prostate cancer that can be treated with active surveillance?
Risk factors can be assessed to determine a man’s risk category to see if he is a candidate for active surveillance. Men are characterized as having low, medium or high-risk disease.
Those with low risk disease are often candidates for active surveillance. Men with low risk disease, and who may meet criteria for active surveillance include low stage (T1 or T2a), Gleason score 6 or less (and no evidence of Gleason 4 subtype, unless small volume in men over 70), less than one third of the biopsies showing cancer, and no more than 50% of any one core showing cancer
Again, information from the AUA Guidelines notes, “Which patients are suitable candidates for active surveillance? Patients with lower risk tumors (low Gleason score, PSA level, and clinical stage) could be candidates for this treatment strategy. Several studies have shown that patients with lower grade, localized prostate cancer have a low risk for clinical progression within the first 10 to 15 years after the diagnosis. This treatment strategy may be best suited for men with a shorter life expectancy. Generally, patients with high-grade tumors have a relatively poor prognosis and are not suitable for active surveillance.”
Is there additional information that helps assess risk?
In more recent years, additional information is available to help assess the potential aggressiveness of the cancer. While stage (anatomic extent), grade (Gleason score) and volume (amount of disease) are the most important factors to identify risk group, genetic testing of the biopsy material (e.g., Polaris or Decipher test) is now available to identify certain genes which may suggest either an increase or decrease in the aggressive potential of the cancer cells. The additional information provided with genetic testing may help determine if a man is a suitable candidate for active surveillance, or whether he should consider undergoing intervention with either surgery or radiation. Also, prostate imaging with multiphase MRI may provide additional information that may help assess the extent of disease to assist with treatment selection.
How are men on active surveillance monitored?
For those men who choose active surveillance, ongoing monitoring includes regular office checkups at six month intervals to include PSA and digital rectal exam (examination of the prostate), with repeat biopsy at 1 to 2 years after the initial diagnosis, and at 3 to 5 year intervals thereafter (or sooner if clinically indicated) .
Take Home Message
Once a man has been diagnosed with prostate cancer, the goal is to make an effort to answer the questions, “What trouble might the disease cause? What is available to help prevent that? What are the burdens and hazards associated with those efforts to help?”
For those men who have disease that is not likely to cause trouble, and for whom the potential hazards and burdens of treatment may outweigh the potential benefit, active surveillance is an appropriate treatment avenue.
Contact us to request an appointment or ask a question. We're here for you.



