Prostate Cancer Brachytherapy
What is brachytherapy?
Radiation therapy is frequently used to treat prostate cancer. One of the commonly used forms of radiation therapy is the insertion of radioactive seeds into the prostate, which is called brachytherapy or interstitial radiation therapy.
Before the advent of seed implant, a man’s choices for addressing clinically localized prostate cancer included radical prostatectomy or external beam radiotherapy. Now, seeds can be used alone or in combination with external beam radiotherapy and hormonal therapy to treat clinically localized prostate cancer. The advantage of seeds compared to external radiation is that it can be carried out as a one-time outpatient based treatment.
Who is a candidate for seed implant?
Several factors determine if a man is a candidate for seed implant. These include the stage and grade of the prostate cancer, the PSA level, and the size of the prostate. Stage refers to the anatomic extent of the prostate cancer (as outlined in the separate Prostate cancer newsletter). Grade refers to the histologic appearance of the prostate cancer cells and glands as visualized microscopically. The Gleason’s score is the most commonly used grading system. Gleason’s scores range from 2 through 10. The prostate size is measured at the time of the ultrasound and biopsy.
To be eligible for seed implant alone, a man should have Stage T1-T2 disease, Gleason score 6 or less, PSA less than 10, and a prostate size less than 50 cc.
Is seed implant the only treatment or is it combined with other treatments?
When these criteria for seed implant alone are not met, then seed implant may be combined with external beam radiotherapy or hormonal therapy in the form of Lupron.
When external beam radiotherapy is used in combination with seed implant, the patient typically receives a 4-5 week course of external beam radiation therapy. Treatments are delivered as an outpatient on a daily basis. Seed implant then follows several weeks after the conclusion of external beam radiotherapy. Alternatively, the seed implant may precede the course of external beam radiotherapy.
In some men hormone therapy, also known as androgen deprivation therapy, is given in the form of Lupron prior to starting treatment with radiotherapy. Prostate cancer depends on testosterone, the male hormone, to grow and to flourish. When testosterone is removed, the prostate cancer cells become quiet. There is some evidence that suggests prostate cancer cells are more sensitive to external radiation when testosterone is absent. There are a variety of ways to improve testosterone on a temporary or permanent basis. One of the most commonly used approaches involves the administration of Lupron. Lupron is an intramuscular injection, which is given in the buttocks. Typically a 6-month Depo Lupron injection is used. After the injection, the body does not make testosterone for the next six months. Without testosterone, the PSA typically declines significantly and the prostate cancer cells become inactive. Effects associated with Lupron therapy include loss of libido (sexual drive and interest) and diminished or absent erection. Hot flashes occur in approximately 50% of the men. These side effects of Lupron typically resolve once the effect of the Lupron has subsided.
Lupron is also used in some men to decrease the size of the prostate. Prostate size is an important factor in selecting a man as a candidate for seed implant. Ideally, the prostate should be less than 50 cc in volume. When the prostate is less than 50 cc, seed implantation is technically easier because the pubic bone is not in the way during the placement of the needles to introduce the seeds. For those men whose prostates are larger than 50 cc in size, pretreatment with Lupron may be carried out to reduce the size of the prostate to make subsequent seed implant easier.
What happens when a man chooses to have a seed implant?
Once the patient decides to proceed with seeds, the next step includes evaluation by a radiation oncologist. The urologist and radiation oncologist jointly decide on the optimum form of therapy for an individual patient. They determine if seeds will be used alone or in combination with external beam radiotherapy and/or hormonal therapy. If hormonal therapy is required, the patient typically receives a Lupron shot first and then begins his subsequent treatment within several months. If external beam radiotherapy is part of the treatment plan, the patient typically receives his 4-5 weeks of external radiation followed by the seed implant procedure.
Preoperative preparation for seed implant is listed on a separate instruction sheet. Antibiotics are started several days in advance of the procedure to reduce the risk of infection. Even though patients are told not to eat or drink after midnight the night before the procedure, they should still take their antibiotic pill with a sip of water on the morning of the procedure itself. Patients are also started on an alpha-blocker to make urination less problematic postoperatively. An alpha-blocker, such as Flomax, Uroxatral, Hytrin or Cardura, is started on a once-daily basis. Alpha-blockers reduce the constriction of the prostate around the urethra. With less constriction, urination is easier with less frequency and urgency.
How is the procedure done?
The actual seed implant is done on an outpatient basis under anesthesia. The surgery center tells the patient when to arrive, which is typically two hours in advance of the procedure. The seed implants takes 1-2 hours. Patients are in the recovery room for several hours after the procedure, following which they are discharged to home. Anywhere from 50-200 seeds may be placed at the time of the seed implant.
The seeds are implanted using needles that are placed through the perineum (this is the area in back of the scrotum and in front of the anus).
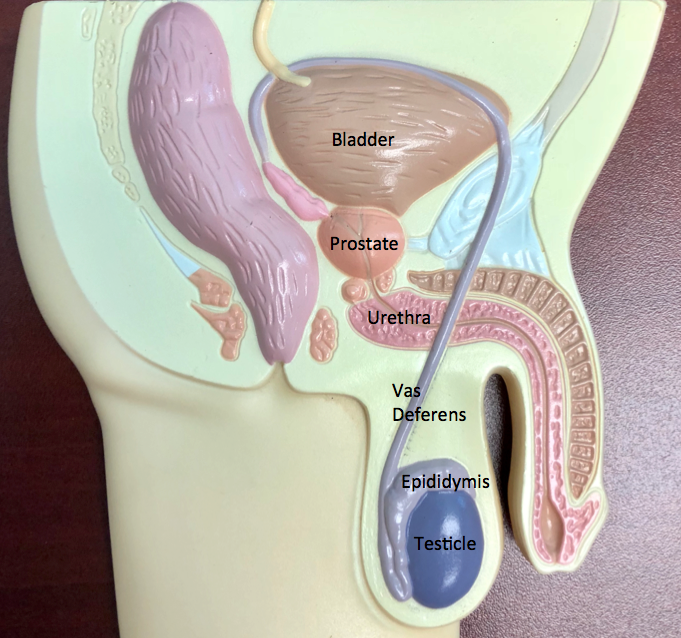
An ultrasound probe is present in the rectum to guide proper needle placement and seed distribution. Seed types commonly used are Iodine 125 and Palladium 103. The choice of seed type is determined on an individual basis.
What happens after the procedure?
After the procedure, patients are allowed to resume their normal activity within the first week. It is normal to see blood in the urine or in the bowels on an intermittent basis for the first several weeks. A follow-up CT scan is done at approximately one month postoperatively. This CT scan, arranged by the radiation oncologist, allows final evaluation of the radiation dose distribution.
What are the hazards of treatment?
Long-term complications associated with the procedure include erectile dysfunction, urinary frequency and urgency, and bowel irritability. Men often retain their ability to have erection at first. However, over ensuing years, as many as 3⁄4 of men lose their erection. Most men notice an increase in frequency and urgency of urination for the first several months after their procedure. Symptoms may persist over time in approximately 10-20% of men. Loose bowel movements and increased frequency of bowel movements may occur during the first several months after treatment. Bowel symptoms, including urgency of bowel movements, may persist in 10-20% of men.
Take Home Message
Currently, seed implant for prostate is a useful treatment avenue. For the right patient, it is a minimally invasive procedure that provides benefit.
Contact us to request an appointment or ask a question. We're here for you.



