Androgen Deprivation Hormone Therapy for Prostate Cancer
What is ADT and Why It Matters
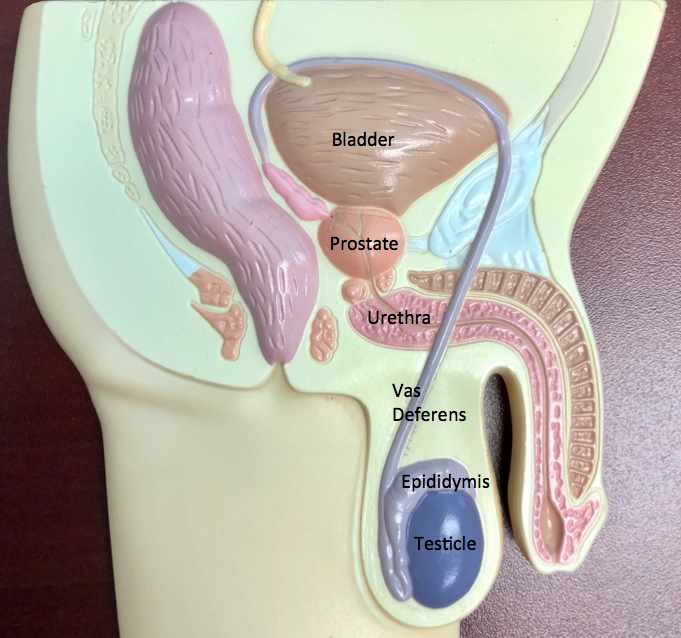
Androgen Deprivation Therapy (ADT) is a treatment that reduces or blocks male hormones (androgens) such as testosterone, which prostate cancer cells rely on to grow. ADT is used to treat prostate cancer at various stages, including intermediate or high-risk localized disease, node-positive disease after surgery, and metastatic disease. By lowering hormone levels, ADT helps slow cancer growth, shrink tumors, reduce symptoms, and extend survival.
At The Urology Group, ADT may be used alone or in combination with other treatments such as surgery, radiation therapy, or advanced hormone therapies, depending on the patient’s diagnosis and treatment goals.
Purpose of ADT
The goal of ADT is to reduce testosterone to very low levels, depriving prostate cancer cells of the stimulation they need to grow. This therapy helps:
- Slow tumor progression and lower PSA levels
- Delay or prevent the spread of cancer
- Improve the effectiveness of other treatments
- Control symptoms in advanced stages of disease
Risks and Side Effects
While ADT is an effective therapy, it can also cause side effects due to reduced testosterone levels. Common effects include:
- Decreased libido and erectile dysfunction
- Hot flashes, fatigue, weight gain, and loss of muscle mass
- Breast tenderness or enlargement
- Mood changes, depression, and decreased mental sharpness
- Increased risk of diabetes, high cholesterol, and cardiovascular disease
- Bone thinning (osteopenia or osteoporosis) and higher fracture risk
Your provider will monitor for these risks and help manage them with lifestyle strategies, medication, and regular health assessments.
Bone Health and ADT
Bone health is an important part of ADT management. Testosterone helps maintain bone strength, and lowering testosterone can cause a decline in bone mineral density. This increases the risk of fractures, especially in the spine and hips.
Patients starting ADT should:
- Receive a baseline bone density (DXA) scan and periodic follow-up testing
- Take vitamin D and calcium supplements as recommended
- Engage in regular weight-bearing exercise and strength training
- Avoid smoking and excessive alcohol
- Discuss bone-protective medications such as bisphosphonates or denosumab if appropriate
At The Urology Group, bone health evaluation is part of every ADT treatment plan. Our providers work with patients to prevent bone loss and protect long-term health.
Medications Used in ADT and Advanced Hormone Therapy
Several medications are available to suppress or block androgens, each with unique benefits and dosing schedules.
Orgovyx (relugolix)
An oral GnRH antagonist that rapidly lowers testosterone levels. Taken daily, it offers a needle-free alternative to injectable hormone therapies.
Camcevi (leuprolide mesylate)
A long-acting injectable GnRH agonist given subcutaneously every three or six months. Used for advanced or recurrent prostate cancer.
Eligard (leuprolide acetate)
A widely used injectable GnRH agonist available in multiple dosing intervals. It suppresses testosterone and is administered by healthcare professionals.
Nubeqa (darolutamide)
An androgen receptor inhibitor used in combination with ADT for certain types of metastatic or non-metastatic prostate cancer. It helps block the action of androgens in cancer cells.
Xtandi (enzalutamide)
Another androgen receptor inhibitor that prevents androgens from stimulating cancer cell growth. Often used with or after ADT in advanced prostate cancer.
Abiraterone (abiraterone acetate) plus prednisone
A combination therapy that blocks androgen production from the testes, adrenal glands, and tumor tissue. It is used with low-dose prednisone to minimize side effects and is indicated for metastatic prostate cancer.
Erleada (apalutamide)
An oral androgen receptor inhibitor used with ADT for non-metastatic and metastatic hormone-sensitive prostate cancer. Erleada blocks testosterone from stimulating cancer growth and has been shown to delay disease progression and extend survival.
Coordinated Care
At The Urology Group, patients receiving ADT are managed through a coordinated care approach. We closely monitor treatment response through PSA levels, imaging, and side-effect management. Our team focuses on maintaining quality of life through attention to bone health, cardiovascular wellness, and overall well-being.
In Office Dispensing of ADT Medications
The Urology Group offers in office dispensing of several androgen deprivation and advanced hormone therapy medications, including Orgovyx, Camcevi, Eligard, Nubeqa, Xtandi, and abiraterone with prednisone. Providing these treatments directly through our offices ensures that patients receive their prescribed therapy quickly, safely, and with coordinated oversight from their care team.
In office dispensing allows our providers and pharmacists to verify dosing, review potential side effects, and reinforce adherence at every visit. This model improves continuity of care and helps patients avoid delays or errors that can occur when prescriptions are filled through outside specialty pharmacies.
Patients benefit from:
- Improved safety: Direct communication between the prescribing provider, pharmacist, and patient ensures accuracy and prompt management of any side effects.
- Better adherence: Patients are more likely to stay on schedule when medications are dispensed and monitored within the practice.
- Coordinated insurance support: Our dispensing team works directly with insurers to streamline prior authorizations and copay assistance, reducing administrative burden for patients.
- Continuity of care: Every dose and response are documented in the patient’s chart, allowing for seamless coordination among providers, nurses, and the Care Management team.
In office dispensing gives patients peace of mind knowing their cancer therapy is handled under one roof by the same trusted team managing their overall treatment plan. This approach enhances safety, adherence, and outcomes, reflecting The Urology Group’s commitment to comprehensive prostate cancer care.
How Our Care Management Program Helps
The Urology Group’s Care Management Program provides ongoing, personalized support for patients undergoing cancer treatment, including those receiving ADT. Our dedicated care coordinators work closely with patients to:
- Monitor for side effects such as fatigue, mood changes, and bone loss
- Coordinate lab tests, imaging, and follow-up appointments
- Reinforce medication adherence and dosing schedules
- Provide education on nutrition, exercise, and cardiovascular health
- Connect patients with resources for emotional and mental well-being
This proactive approach ensures patients have the support they need between office visits, helping them stay on track, reduce complications, and maintain their overall health during therapy. Call (703) 936-2922 today to enroll in our Care Management program.
Our Commitment
ADT remains a cornerstone of prostate cancer management. At The Urology Group, we are committed to providing comprehensive, personalized care to help patients understand their treatment, manage side effects, and maintain quality of life.
References
Centers for Disease Control and Prevention. Prostate Cancer Treatment: Hormone Therapy. 2025. cancer.gov/types/prostate/prostate-hormone-therapy-fact-sheet
Mayo Clinic. Hormone Therapy for Prostate Cancer. Reviewed July 2025. mayoclinic.org/tests-procedures/hormone-therapy-for-prostate-cancer/about/pac-20384737
Greenspan SL, et al. Bone Health in Men Receiving Androgen Deprivation Therapy for Prostate Cancer. Can Urol Assoc J. 2012;6(6):E328-E334.
Huynh C. Osteoporosis from Androgen Deprivation Therapy in Prostate Cancer. RACGP. 2010.
JAMA Network Open. Association of Bone Mineral Density Testing With Risk of Major Fractures in Prostate Cancer Survivors Treated With ADT. 2023.
ADT, androgen deprivation, hormone therapy, testosterone, prostate cancer, Orgovyx, Camcevi, Eligard, Nubequa, Xtandi, Abiaterone, Erleada
Print PageContact us to request an appointment or ask a question. We're here for you.



