Urinary Incontinence
Urinary incontinence is a condition that affects both men and women. Some estimates suggest that one out of three women may have some form of incontinence. Incontinence is a term used to describe the involuntary loss of urine.

Urinary incontinence is a condition that affects both men and women. Some estimates suggest that one out of three women may have some form of incontinence. Incontinence is a term used to describe the involuntary loss of urine.
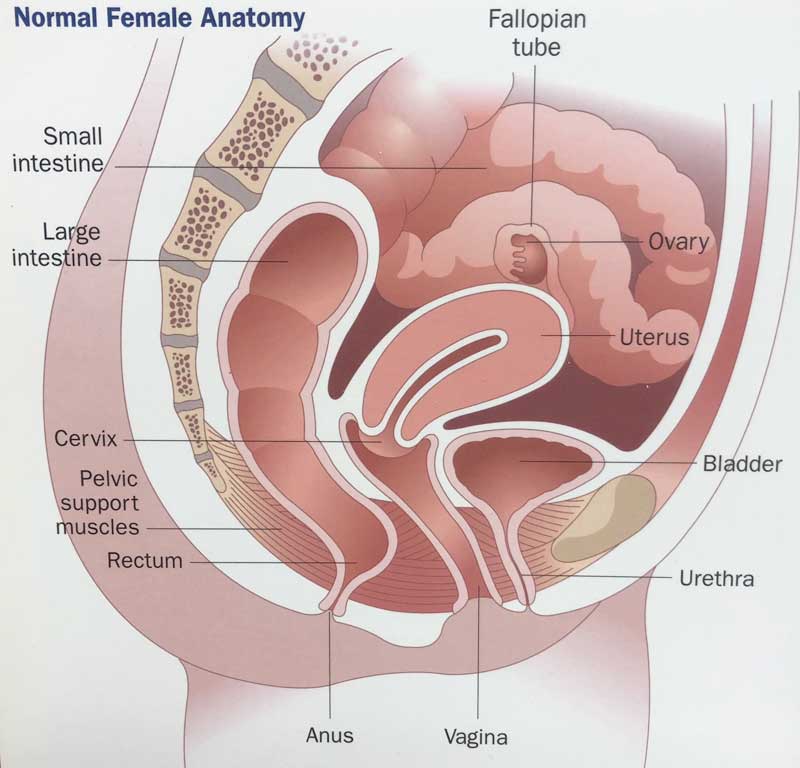
To understand incontinence, it helps to understand how the urinary system works. Urine is made in the kidneys. The kidneys, which sit high in the back under the rib cage, filter the blood and extract excess waste products and fluid to form the urine. The urine, once made in the kidneys, travels down a tube on each side called the ureter until it reaches the bladder. The bladder stores urine until full and then it empties urine to the outside through the urethra.
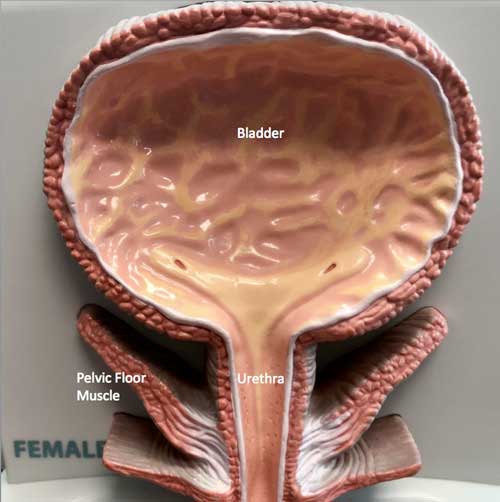
Incontinence occurs when the bladder does not store urine properly. In general, there are two common types of incontinence – stress incontinence and urge incontinence. Stress incontinence occurs when there is a sudden increase in pressure to the bladder, such as that which occurs with coughing, sneezing, running, dancing, or changing from sitting to standing position. This sudden increase in pressure, known as a “stress” to the bladder, causes urine to leak from the bladder through the urethra. The other type of incontinence is urge incontinence. Urge incontinence occurs when there is the sudden sense of the need to urinate but the inability to postpone voiding to reach the bathroom in time. In that circumstance, the bladder begins to contract on its own such that urine is lost involuntarily.
Stress incontinence usually occurs as a result of weakening of the support structures in the pelvis that hold up the bladder and urethra. Childbirth and menopause are two factors that may contribute to a woman’s chance of developing stress urinary incontinence. In men, stress incontinence may develop as a result of prostatic surgery.
The examination for incontinence includes checking the abdomen and groin areas. The position of the bladder and urethra are checked. In women, an internal exam may be done to determine if there is anything pressing on the bladder and urethra.
In addition to the office examination, a urodynamic study may be done. Urodynamics refers to tests done to measure the capacity of the bladder and the pressures at which urinary leakage takes place. These tests are done by placing a small catheter into the bladder. The bladder is then filled to evaluate its storage ability and to identify the pressure at which leakage takes place.
Stress incontinence is managed with a stepwise approach. Kegel exercises are usually tried as part of the initial management. These are done by squeezing the muscles of the pelvic floor for 5-10 seconds at a time for 30-40 times a day. The “right” muscles to exercise are identified by contracting the muscle during urination that stops the flow of urine. Once that muscle is identified, it should be exercised 30-40 times during the day when not urinating. For example, it can be done while riding in a car, sitting in a chair, or standing in a store. The muscle does not need to be squeezed during urination on a regular basis. Kegel exercises lessen stress incontinence in about half of patients, but the effect may not be noticeable until after 3-4 months of carrying out these exercises.
Other non-surgical methods occasionally help with stress incontinence. Pelvic floor stimulation and biofeedback may offer some benefit. In postmenopausal women, vaginal Premarin cream may help restore some tone to the pelvic floor supporting structures and lessen symptoms of stress urinary incontinence.
If the above methods are not providing benefit and if the symptoms are troublesome enough that a patient wants something done, surgical techniques are available to address stress urinary incontinence. In some patients with stress urinary incontinence, leakage develops due to failure of the urethra to close tightly. In this case, collagen can be injected underneath the surface of the urethra to create a better seal. This technique is carried out on an outpatient basis with minimal sedation. Many patients notice a favorable initial improvement. However, the collagen becomes reabsorbed in most and the results provide short-term help only.
In men, a device called an artificial urinary sphincter may be placed around the urethra which may lead to resolution of urinary leakage.
In women, a variety of different procedures are available. In the past, surgery required an operation in the lower abdomen. An effort was made to attach the bladder or urethra to the undersurface of the pelvic support structures. Patients were usually in the hospital for several days postoperatively and oftentimes required a catheter (a tube to drain the bladder) for a week or more.
Current techniques in women use a “sling” to restore support to the bladder and urethra. A small vaginal incision is used to place the sling underneath the urethra. The sling works like a hammock to hold to the urethra in the proper place. These procedures can be done on an outpatient basis and usually do not require a catheter postoperatively. Over 90% are completely dry or dry most of the time. However, time and gravity remain the enemies and urinary leakage may recur in the future. Complications with any type of surgery include bleeding or infection, as well as the general risks of surgery.
Urge incontinence refers to urinary loss that occurs when there is the sudden urge to void and the inability to reach the bathroom in time. Urge incontinence occurs because the bladder involuntarily contracts on its own to push urine to the outside. If the bladder had its way, it would never fill with urine and would contract as soon as urine reached the bladder from the kidney. However, the bladder is prevented from going on its own by a reflex. When the reflex does not work properly, the bladder has an “uninhibited contraction” and goes on its own. Patient who have urge incontinence say they are plagued with situations where they may reach the door of their house and feel an intense need to go, but before they can get the door unlocked and reach the bathroom, they begin to get wet.
A variety of medications are available to manage urge incontinence and include Detrol, Ditropan, Enablex, Oxytrol, VESIcare, and Sanctura. These medications suppress “uninhibited bladder contractions” and lessen the likelihood of the bladder going on its own.
Some patients have a mix of both stress and urge incontinence and a combination of the above treatments may be used.
In summary, incontinence is a common problem. With appropriate evaluation and treatment, many patients can be helped.
Print PageContact us to request an appointment or ask a question. We're here for you.