Prostatitis
Prostatitis is a term used to describe inflammatory and infectious conditions of the prostate. The prostate is a gland that is part of the reproductive system that is closely associated with the urinary tract.
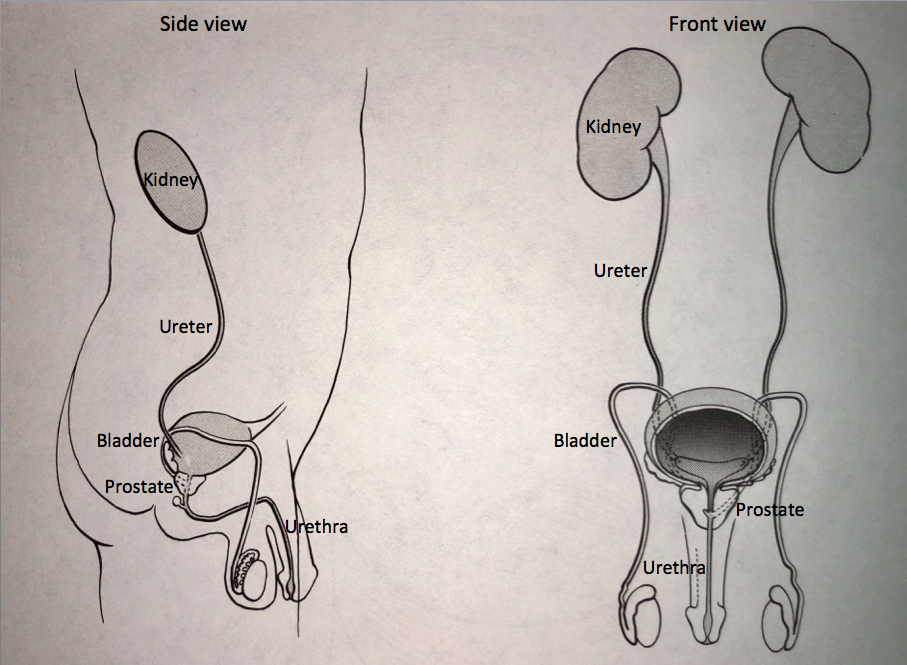
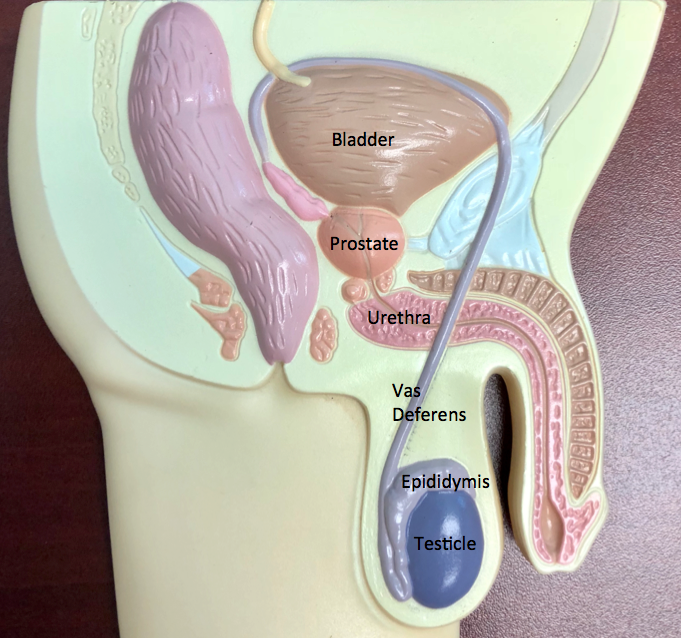
How is the urinary system put together? What is the prostate?
The urinary system begins with the kidneys, which sit high up in the back. The kidneys filter the blood and take out the excess fluid and waste products and form the urine. Urine once formed in the kidney travels through a tube on each side called the ureter down to the bladder. The bladder sits in the lower part of the abdomen. The bladder stores the urine until full and then empties the urine to the outside through the urethra, which is the urinary channel that runs through the penis. The prostate wraps around the urethra at the junction of the bladder and the urethra.
As noted above, the prostate is part of the reproductive system. The reproductive system begins with the testicles, which are in the scrotum. They make the sperm that is carried through a tube on each side called the vas deferens (this is what is divided when a person has a vasectomy). The sperm comes through the vas deferens and mixes with the fluid from the seminal vesicles and prostate to form the semen. The semen is the fluid that comes out at the time of ejaculation. The prostate makes a portion of the fluid that forms the semen.
What is Prostatitis?
Prostatitis is the term used to describe inflammation in the prostate.
Acute prostatitis refers to the sudden onset of a urinary tract infection that also involves the prostate gland. It often occurs in association with high fever and typically responds well to antibiotic treatment.
Chronic prostatitis refers to ongoing inflammation of the prostate gland.
Prostatodynia refers to pain and discomfort originating in the pelvic area that is not associated with prostate infection but is more likely due to spasm of the muscles of the pelvic floor.
What are the symptoms?
Symptoms of prostatitis can include lower abdominal or pelvic ache and a sense of discomfort in the testicles or in the rectal area.
Pain may also be present in the area behind the scrotum and in front of the rectum. Sometimes there can be an uncomfortable sensation in this area that occurs while sitting. There can even be a sensation of “sitting on a golf ball.” Because the prostate wraps around the urethra, urinary symptoms may be present as well. These can include urinary frequency (the need to urinate more often) urgency (the need to urinate as soon as one gets the urge) and nocturia (the need to urinate frequently at night). Burning and stinging with urination may be present as well.
How is a man evaluated to see if prostatitis may be present?
The physical examination begins with inspection of the abdomen and groin area. Then a digital rectal examination is done to feel the surface of the prostate. The physician inserts a gloved finger into the rectal area to feel the prostate to make sure there are not any abnormalities such as prostate cancer. On some occasions the prostate may be “massaged” which means mild pressure is applied while examining the prostate to express prostatic fluid into the urethra. Occasionally, this fluid comes out from the tip of the penis. Alternatively, the patient may be asked to void after the examination to wash out this fluid with the urine. These samples can be inspected under the microscope to determine if inflammatory cells are present. As part of the examination a PSA is often done. This is a blood test done to check for prostate cancer.
Goals of treatment – first make sure nothing bad; second try to lessen symptoms (if possible)
The natural history of prostatitis is that it may recur intermittently over time. However, it does not pose a long-term risk to one’s health. It does not lead to kidney problems or prostate cancer. The primary goal of evaluation is to confirm that the findings are consistent with chronic prostatitis or prostatodynia and to exclude other possible causes of the above symptoms. Once the diagnosis is confirmed, then the main goal is symptom control. The key components of symptom control include anti-inflammatory medication, hot baths and dietary avoidance.
Print PageContact us to request an appointment or ask a question. We're here for you.




