Vasectomy Information
What is a vasectomy?
Vasectomy is one of the most common and popular forms of birth control for those whose families are complete. Vasectomy is a procedure designed to make a man sterile, which means he will not be able to make a female partner pregnant. To understand vasectomy, it helps to understand how the male reproductive system works. The male anatomy is shown in the picture. The scrotum, or sac, contains a testicle on each side.
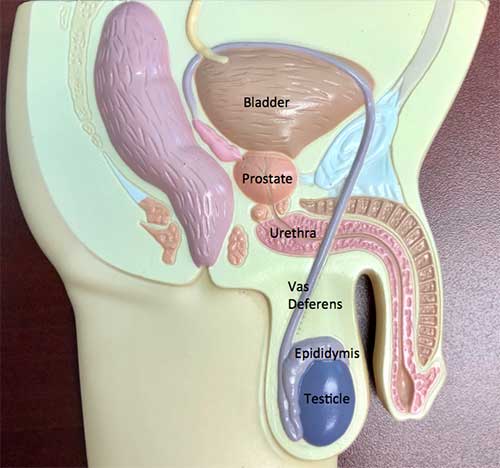
The testicle has two functions. It makes testosterone, the male hormone, which is absorbed into the blood stream. It also makes sperm which travels from the testicle into a series of tubes which collectively form the epididymis. The epididymis sits to the side and in back of the testis. Sperm leaves the epididymis by way of the vas deferens (this is the tube that is divided during a vasectomy) which travels to join the seminal vesicles and prostate. Sperm mixes with fluid from the seminal vesicles and prostate to produce semen, the fluid that comes out from the penis at the time of ejaculation.
At vasectomy, the vas deferens is divided. An approximately half-inch segment of the vas deferns tube is removed. The divided ends are then tied with suture and the ends are sealed shut with cautery or heat. Sperm is still made in the testicle but it cannot get through the block. The testes reabsorb the sperm. The testes do not “back up” or become swollen. Sexual function remains the same. Men still get a normal erection, have a climax, and fluid (semen) still comes out. However, after a period of time – usually about two months – there is no longer any sperm present in the semen that is ejaculated.
Patient comfort. Patient safety. Latest techniques. Broad and extensive experience. The Urology Group provides men the opportunity to undergo vasectomy in a safe, comfortable environment under the hands of an experienced surgeon.”
Experience and Clinical Expertise
Our vasectomy specialists bring together long-standing experience and clinical expertise to make vasectomy a safer and easier procedure for men. Vasectomy has become one of the most popular options available for those whose families are complete, yet many men are anxious about the idea of vasectomy. As men say, they worry about having surgery in “such a sensitive area”.
At The Urology Group we specialize in the latest surgical techniques combined with intravenous sedation in the safest environment to make vasectomy a safe and comfortable experience. We start with our group of doctors, each of whom is a Board certified urologist with extensive operative experience and clinical expertise. Our doctors are part of The Urology Group, a growing, thriving practice first started in 1924, with an 95+ year history of compassionate care and clinical excellence. More importantly, we have extensive experience with vasectomy and have done innumerable vasectomy procedures. We currently perform more than 1,000 vasectomies each year. This vast clinical experience keeps our skills up to date, providing patients with the doctors they want – skilled, competent surgeons. We currently perform the no scalpel vasectomy procedure which is less invasive than prior techniques and provides for a more favorable recovery.
In addition to our surgical expertise, we add in our collaboration with the outpatient surgical centers to provide the extra margin for patient safety. We find that intravenous sedation and monitored anesthesia care under the direction of Board certified anesthesiologists makes our patients comfortable so that they do not “feel anything” during the procedure itself. State of the art monitoring is used to maximize patient safety. We have moved well beyond the old days of local anesthesia in the office and a doctor’s advice to “hold on, you may feel this a little bit”.
Contrary to what many people think, a man is not sterile immediately after the procedure. Sperm are present above the site where the vas is divided. Until these sperm cells have been released in subsequent ejaculations, a man is still fertile and capable of producing pregnancy. Typically, it takes several months after vasectomy for the remaining sperm above the block to be ejaculated. A semen sample must be checked two to three months postoperatively to determine if any sperm are left. Until the semen sample shows no sperm left, a couple must continue with another form of birth control.
Yes. For all intents, a man should be considered permanently sterile. The chance of the two ends “rejoining” is about 1 in 200. The divided ends of the vas do not actually grow back together. Rather, sperm, which are active swimmers, can escape from one end of the vas and find their way into the other end. If this happens, so called “recanalization”, it is most likely to occur within the first several months after the procedure. That is an additional reason to wait until at least two months after the vasectomy procedure to check the semen analysis to determine if there are any sperm left.
The divided end of the vas can be rejoined, a so called vasectomy reversal or vasectomy reanastomosis. However, vasectomy reversal is a more complex procedure than vasectomy. The channel within the vas deferens is so small that it cannot be seen with the naked eye. When vasectomy reversal is carried out, it is done under an operating microscope with 20-fold magnification using suture that can be seen only under a microscope. Even when the ends of the vas deferens are successfully rejoined surgically, the success rate for subsequent pregnancy is less than half. As such, vasectomy should be considered a permanent procedure for those whose families are complete.
Although vasectomy makes a man sterile, it does not affect potency – the ability to have an erection and reach climax. Many couples find that their sex life improves after vasectomy because they no longer worry about the surprise of unwanted pregnancy.
Yes. Most of the seminal fluid which a man ejaculates during intercourse is produced by the seminal vesicle and the prostate gland. Only a small amount of the seminal fluid consists of sperm. After vasectomy, ejaculation remains the same. There typically is a decrease in the amount of fluid ejaculated, but for most men this difference is barely noticeable.
In years past, when anesthesia choices were limited, vasectomy was done using local anesthesia only. For as many as half the men, vasectomy was an uncomfortable procedure. With the advent of improved anesthesia techniques and the development of outpatient surgical centers, current practice favors use of a combination of local anesthesia with IV sedation so that men are in a “twilight” state, where they do not feel anything at all during the procedure. In addition to improved anesthesia techniques, vasectomy is currently done with the no scalpel technique, which is much less invasive. In years past, a large incision was required on each side of the scrotum to gain access to the vas deferens. Currently, a small puncture site is made in the scrotum to bring the vas up to the outside where the vasectomy can be performed. The less invasive nature of this procedure make for an easier operative course and postoperative recovery.
Potential risks include bleeding and infection which occur in less than 1% of the men. There will be some pain and tenderness in the area where the surgery is performed. There may also be some swelling and discoloration (black and blue marks). Patients typically feel best if they take two Tylenol every three hours while awake for the first 3-4 days after the procedure. Patients are also given a prescription for pain medication to use in addition to the Tylenol as needed to keep the post-procedure discomfort to a minimum.
As far as medical science can determine at this time, there are no long-term complications associated with vasectomy. Past reports in the lay press have focused attention on scientific studies which raised the question of an increased risk of heart disease or an increased risk of prostate cancer. The current consensus is there is no link between vasectomy and other health conditions.
Men may resume normal sexual activity 1-2 weeks after surgery. The couple should continue to use some other form of contraception until the semen sample shows no sperm left.
Men typically have a vasectomy procedure on a Thursday or a Friday and take the weekend off. By Monday, they can return to work. They should wait two weeks before resuming strenuous activity, such as running, weightlifting, lawn work, and so forth. An athletic supporter is placed at surgery and can be worn for the first 24-48 hours after the operation. After that, either an athletic supporter or brief-style underpants can be worn as needed to provide comfort. A shower may be taken on the day following the procedure. There may be some discharge or drainage from the puncture site, which is normal. A small piece of gauze may be placed over the puncture site as needed to keep the drainage from soiling the clothes. Oftentimes, the puncture site does not require a stitch to be closed. If a stitch is present, it will typically dissolve over the course of the next 1-3 weeks which means there are not stitches which need to be removed later. Black and blue or swelling will typically subside over the course of 1-2 weeks.
In summary, vasectomy is a common procedure that works well for those whose families are complete.
Additional Information
Vasectomy Post-Op Instructions
Vasectomy 2 Week Post-Op Instructions
Contact us to request an appointment or ask a question. We're here for you.




